⚠️ Male Infertility: Common Conditions That Affect Sperm — And What Can Be Done
🔹 Introduction: When Sperm Struggles Have a Medical Cause
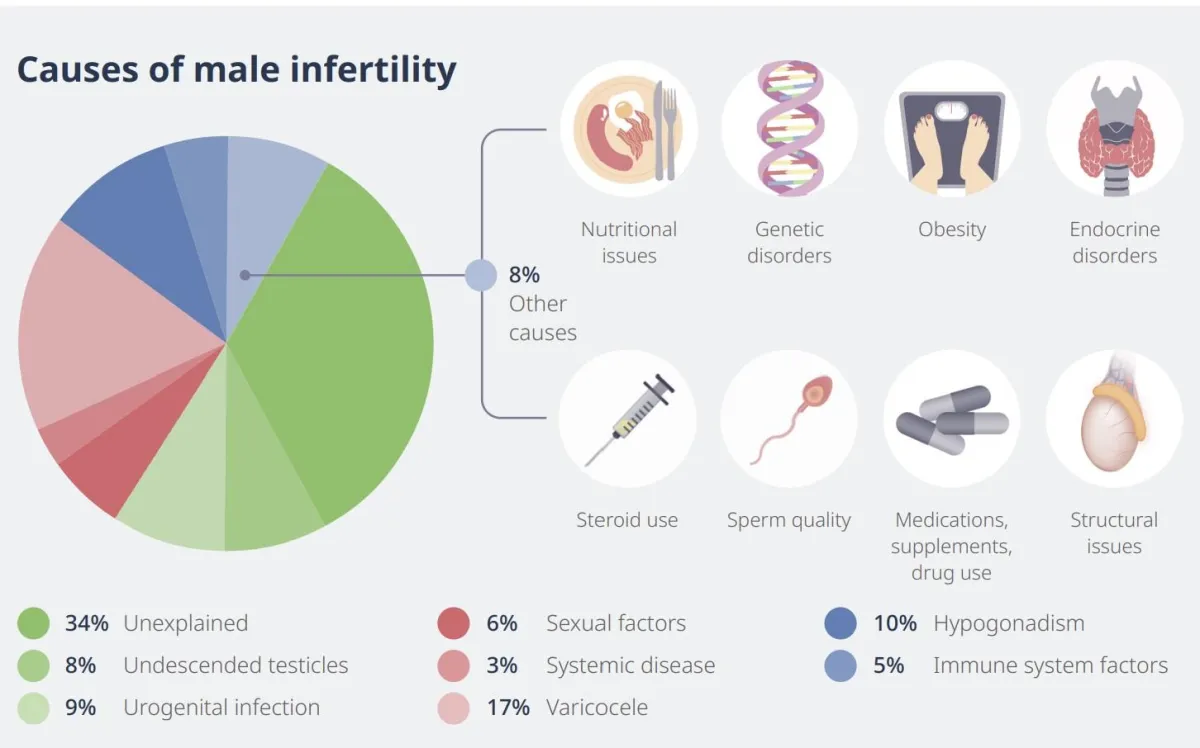
While lifestyle and environment play a big role in sperm health, many men experience fertility issues due to underlying medical conditions. Some are inherited, others acquired — but all of them can impact sperm production, function, or delivery.
The good news? In many cases, there are treatments or procedures that can improve fertility or assist with conception.
🔬 Common Medical Causes of Male Infertility
1. Varicocele (Dilated Testicular Veins)
What it is: Enlarged veins in the scrotum (like varicose veins)
Why it matters: Increases scrotal temperature, leading to DNA fragmentation and reduced sperm count/motility
Symptoms: May feel like a “bag of worms”; often painless
Diagnosis: Physical exam, scrotal ultrasound
Treatment:
Varicocelectomy (surgical repair)
Can improve sperm quality in 30–50% of men within 6–12 months
2. Obstructive Azoospermia
What it is: A complete absence of sperm in semen due to a physical blockage
Causes:
Prior vasectomy
Congenital bilateral absence of the vas deferens (common in men with CF gene)
Scarring from infection or trauma
Diagnosis: Semen analysis + scrotal or transrectal ultrasound
Treatment Options:
Sperm retrieval: TESA, PESA, MESA, or Micro-TESE
IVF with ICSI using retrieved sperm
3. Hormonal Imbalances
What it is: Disruption in hormone signals between brain and testicles
Causes: Pituitary tumors, low FSH/LH, anabolic steroid use, obesity
Diagnosis: Bloodwork: FSH, LH, testosterone, prolactin
Treatment:
Stopping steroids
Medications like clomiphene citrate, aromatase inhibitors, hCG injections
4. Genetic Conditions
Examples:
Klinefelter Syndrome (XXY): Low testosterone, high FSH/LH, small testes
Y chromosome microdeletions: Missing sperm production genes
Diagnosis: Karyotype + Y-chromosome microdeletion testing
Treatment:
Some men can undergo micro-TESE to retrieve sperm directly from testicles
Genetic counseling recommended
5. Infections or STIs
Examples:
Epididymitis, prostatitis, mumps orchitis
Impact: Inflammation can damage sperm-producing structures or block ducts
Diagnosis: Semen culture, urinalysis
Treatment:
Antibiotics, anti-inflammatory meds
Treating underlying STI (e.g., chlamydia)
6. Retrograde Ejaculation
What it is: Semen goes into the bladder instead of out through the urethra
Causes: Diabetes, spinal injury, prostate surgery, medications
Diagnosis: Post-ejaculation urine test (sperm in urine)
Treatment:
Medications like pseudoephedrine
Sperm collection from urine + IUI or IVF
🧪 Procedures That Can Help Retrieve or Improve Sperm
These options are often used before or during IVF cycles:
🔹 Sperm Retrieval Techniques
Used in cases of azoospermia or failed ejaculation:
TESA (Testicular Sperm Aspiration)
PESA (Percutaneous Epididymal Sperm Aspiration)
MESA (Microsurgical Epididymal Sperm Aspiration)
Micro-TESE (Microsurgical Testicular Sperm Extraction) – most effective for non-obstructive azoospermia
🔹 Medical Therapies
Used for men with hormonal issues or borderline counts:
Clomiphene citrate (Clomid): Increases FSH/LH
hCG injections: Boost testosterone and sperm
Aromatase inhibitors: Lower estrogen in overweight men
🔹 Lifestyle Changes
Can improve mild-to-moderate male factor infertility:
Quit tobacco, alcohol, or marijuana
Take antioxidant supplements (zinc, CoQ10, L-carnitine)
Treat obesity and manage chronic stress
Avoid heat (hot tubs, laptops, tight clothing)
🧠 Final Thoughts
Male infertility is more common than most couples realize — and often treatable. In fact, up to 50% of IVF cases involve a male factor. A detailed semen analysis and medical evaluation can uncover the root cause and help fertility specialists tailor the most effective plan — whether that’s hormone therapy, retrieval, or assisted reproduction.