Ultrasound Monitorig
for Your IVF Cycle
For IVF monitoring cycles that are out-of-state of your location
To schedule an appointment
Please Call True Health Acupuncture at 702-475-0870
You can also book online on the True Health Acupuncture website.
1535 W Warm Springs, Ste 135
Henderson, Nevada 89014
Testimonials

Michelle A.
My name is Michelle Aukerman. And I just have to say that Joyce at True Health Acupuncture is probably the best ultrasound technician I have ever had in my life and I’ve been through several. She’s very personal and talks through everything and if something goes wrong, she says OK how do we make this right? What’s the next step we need to take? You don’t hear that from any other ultrasound tech, they're so jaded. The comfort environment at True Health Acupuncture is unmatchable. It does not feel like a doctor's office and everybody is so warm but when it comes to Joyce, she is completely unmatched. It’s like having your own mother right there with you. I highly highly recommend her.
Thank you, the Aukerman’s
This is the second pregnancy that I came to Joyce for my outside monitoring. I have been very nervous about the whole process, but Joyce guided me through each and every ultrasound. Although the monitoring went smoothly, upon achieving pregnancy I developed some bleeding. Of course, I panicked. Joyce explained everything that was going on with my bleeding and helped me through this anxious time. I don’t know what I would have done without Joyce’s calm demeanor. And the added bonus is having acupuncture treatment right there at True Health Acupuncture, the office Joyce works out of. I will always be truly thankful for the amazing experience that I received from both Joyce and True Health to be a part of my fertility journey.

Sara P.
Joyce is an exceptional individual who made a significant impact during my IVF journey. I had the privilege of meeting her when I needed support, and she was able to perform ultrasounds when our IVF Dr was unable to accommodate us. Her ability to confirm our twin pregnancy was incredibly reassuring. Joyce took the time to explain everything she was observing, which not only made the experience more memorable but also helped alleviate my anxiety. Her compassionate approach truly made a difference in my experience.

Nicole B
The Impact of Endometrial Thickness on Blastocyst Implantation
The Impact of Endometrial Thickness on Blastocyst Implantation
In the realm of assisted reproductive technology (ART), the thickness of the endometrium—the lining of the uterus—plays a pivotal role in the successful implantation of a blastocyst. While much attention has been given to the challenges posed by a thin endometrium, it's equally important to understand the implications of an excessively thick endometrial lining on implantation outcomes.
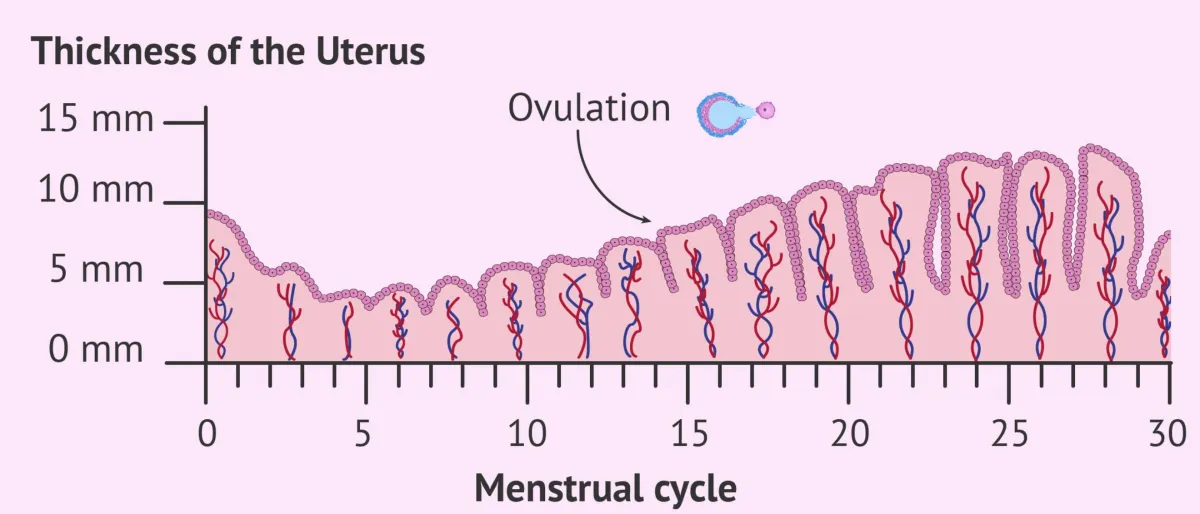
Understanding Endometrial Thickness and Implantation
The endometrium undergoes cyclic changes, thickening in response to hormonal signals to prepare for potential embryo implantation. An optimal endometrial thickness is crucial for implantation success. Recent studies have sought to delineate the relationship between endometrial thickness and live birth rates.
A comprehensive study published in Fertility and Sterility examined over 40,000 fresh and frozen-thaw IVF cycles. The findings indicated that in fresh embryo transfers, live birth rates increased with endometrial thickness up to 10–12 mm. Beyond this range, the rates plateaued, suggesting no additional benefit with further thickening. In frozen embryo transfer cycles, live birth rates improved with endometrial thickness up to 7–10 mm, after which they stabilized. Notably, the study did not find a significant decline in live birth rates with very thick endometrial linings, but the plateau indicates a threshold beyond which increased thickness does not enhance outcomes.
Pharmaceutical Agents Used to Enhance Endometrial Thickness
In IVF protocols, certain pharmaceutical agents are employed to promote endometrial growth, aiming to achieve the optimal thickness for implantation:
Estrogen Therapy: Estradiol valerate is commonly administered to stimulate endometrial proliferation. Studies have shown that this treatment can effectively increase endometrial thickness and improve clinical pregnancy rates.
Sildenafil Citrate (Viagra): Originally used for erectile dysfunction, sildenafil has been utilized off-label to enhance uterine blood flow, thereby potentially increasing endometrial thickness. Clinical trials have reported improvements in endometrial lining and pregnancy outcomes with its use.
Granulocyte Colony-Stimulating Factor (G-CSF): Administered intrauterinely, G-CSF has been explored as a treatment for thin endometrium, showing promise in increasing endometrial thickness and improving implantation rates.
Visualizing the Data
To better understand the relationship between endometrial thickness and implantation success, consider the following chart adapted from recent studies:
Uterine Lining Thickness and Implantation Rates

Conclusion
Achieving an optimal endometrial thickness is a delicate balance in the IVF process. While a lining that's too thin is known to hinder implantation, excessively thick endometrium does not necessarily equate to higher success rates and may plateau in benefit. Personalized treatment plans, often incorporating pharmaceutical agents to modulate endometrial thickness, are essential for optimizing implantation outcomes. Continuous research and individualized patient care remain paramount in enhancing the efficacy of ART procedures.
Starting your cycle
Starting an IVF cycle is stressful enough, doing it with an out-of-state provider just increases that stress. That is why we have developed an out-of state monitoring program to help women that need ultrasound monitoring without having to travel to their provider. We follow your physicians instructions and with be able to accommodate your schedule. Most all cycles, whether retrievals or transfers, will need 2-3 ultrasounds during that cycle. All reports can be faxed or emailed to your physician within 2-3 hours after the exam is finished.