Ultrasound Monitorig
for Your IVF Cycle
For IVF monitoring cycles that are out-of-state of your location
Starting your cycle
Starting an IVF cycle is stressful enough, doing it with an out-of-state provider just increases that stress. That is why we have developed an out-of state monitoring program to help women that need ultrasound monitoring without having to travel to their provider. We follow your physicians instructions and with be able to accommodate your schedule. Most all cycles, whether retrievals or transfers, will need 2-3 ultrasounds during that cycle. All reports can be faxed or emailed to your physician within 2-3 hours after the exam is finished.
To schedule an appointment
Please Call True Health Acupuncture at 702-475-0870
You can also book online on the True Health Acupuncture website.
1481 W Warm Spring Rd #129
Henderson, Nevada 89014
Testimonials
My name is Michelle Aukerman. And I just have to say that Joyce at True Health Acupuncture is probably the best ultrasound technician I have ever had in my life and I’ve been through several. She’s very personal and talks through everything and if something goes wrong, she says OK how do we make this right? What’s the next step we need to take? You don’t hear that from any other ultrasound tech, they're so jaded. The comfort environment at True Health Acupuncture is unmatchable. It does not feel like a doctor's office and everybody is so warm but when it comes to Joyce, she is completely unmatched. It’s like having your own mother right there with you. I highly highly recommend her.
Thank you, the Aukerman’s

Michelle A.
This is the second pregnancy that I came to Joyce for my outside monitoring. I have been very nervous about the whole process, but Joyce guided me through each and every ultrasound. Although the monitoring went smoothly, upon achieving pregnancy I developed some bleeding. Of course, I panicked. Joyce explained everything that was going on with my bleeding and helped me through this anxious time. I don’t know what I would have done without Joyce’s calm demeanor. And the added bonus is having acupuncture treatment right there at True Health Acupuncture, the office Joyce works out of. I will always be truly thankful for the amazing experience that I received from both Joyce and True Health to be a part of my fertility journey.

Sara P.
Joyce is an exceptional individual who made a significant impact during my IVF journey. I had the privilege of meeting her when I needed support, and she was able to perform ultrasounds when our IVF Dr was unable to accommodate us. Her ability to confirm our twin pregnancy was incredibly reassuring. Joyce took the time to explain everything she was observing, which not only made the experience more memorable but also helped alleviate my anxiety. Her compassionate approach truly made a difference in my experience.

Nicole B
What’s Next in IVF — Future Trends and Cutting-Edge Innovations
As IVF enters its fifth decade, science continues to push boundaries. New technologies are making fertility treatment more personalized, more precise, and in some cases, more affordable. In this final section, we explore the most promising innovations reshaping IVF — and what they may mean for patients in the next 5–10 years.
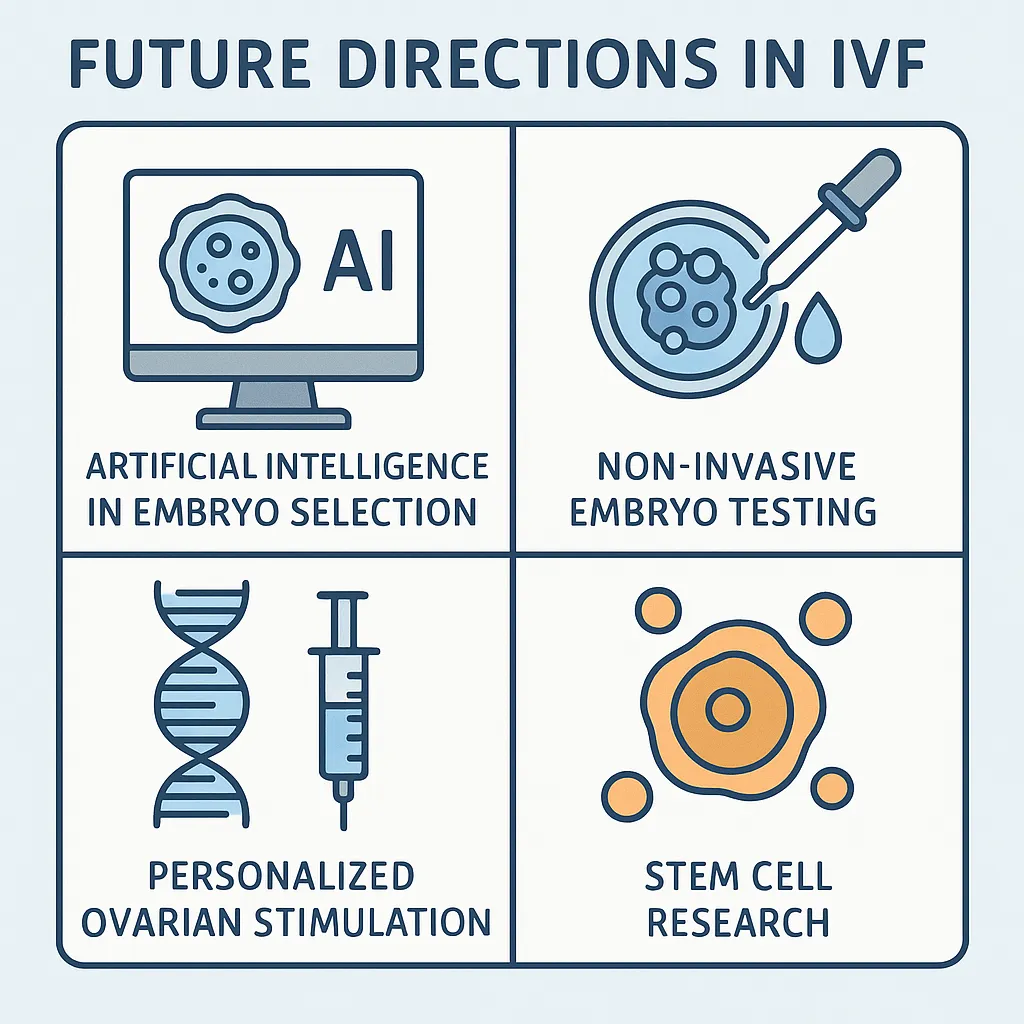
🔹 1. Artificial Intelligence (AI) in Embryo Selection
How it works:
AI-powered platforms analyze time-lapse images of developing embryos to predict implantation potential — sometimes more accurately than the human eye.
Benefits:
Reduces subjectivity in grading
May improve selection of embryos for eSET
Speeds up lab workflow and consistency
Platforms to watch:
Life Whisperer™, iDA Score™, CHLOE EQ™
Status:
Used in some U.S. and international clinics; more studies underway.
🔹 2. Non-Invasive Embryo Testing (niPGT-A)
What it is:
Instead of biopsying cells from the embryo, niPGT-A analyzes DNA shed into the surrounding culture medium during blastocyst development.
Potential Advantages:
No damage to embryo
Easier lab technique
Reduces risk of false results due to mosaicism
Limitations:
Still experimental
Less DNA available; accuracy varies
🔹 3. Personalized Ovarian Stimulation (Pharmacogenomics)
Concept:
Using your genetic profile to determine the best stimulation drugs and doses.
Benefits:
Reduces trial-and-error cycles
May improve response in poor or hyper-responders
Avoids overmedication
Example:
Some clinics now offer AMH + FSHR gene testing before IVF protocols.
🔹 4. Stem Cell Research and Ovarian Rejuvenation
Emerging ideas:
Using stem cells or platelet-rich plasma (PRP) injections into the ovaries to regenerate follicle growth.
Goal: Help women with diminished ovarian reserve, early menopause, or chemo-related infertility.
Status:
Early clinical trials in Europe and Asia. Not standard of care in the U.S.
🔹 5. Uterine Environment Optimization
New efforts are being made to:
Profile the endometrial microbiome (healthy vs. inflammatory bacteria)
Time transfers using endometrial receptivity assays (ERA)
Reduce immune rejection via targeted therapies
These aim to increase the chance of implantation — especially in recurrent failure cases.
🔹 6. IVF Lab Automation and Mini-IVF Clinics
Some labs are automating embryo culture and analysis using:
Automated incubators
Robotic ICSI injectors
Remote monitoring
At the same time, smaller clinics offering affordable Mini-IVF or IVF-in-a-box kits are becoming available — especially for underserved or rural patients.
✅ Looking Ahead: IVF is Becoming Smarter, Gentler, and More Personalized
Innovation Goal AI embryo selection More precise embryo choice Non-invasive PGT-A Safer embryo testing Genetic profiling Better drug selection PRP and stem cells Ovarian rejuvenation Lab automation Consistency and access
These tools promise to enhance outcomes, reduce side effects, and personalize care, especially for patients who have struggled with traditional IVF.