Ultrasound Monitorig
for Your IVF Cycle
For IVF monitoring cycles that are out-of-state of your location
Starting your cycle
Starting an IVF cycle is stressful enough, doing it with an out-of-state provider just increases that stress. That is why we have developed an out-of state monitoring program to help women that need ultrasound monitoring without having to travel to their provider. We follow your physicians instructions and with be able to accommodate your schedule. Most all cycles, whether retrievals or transfers, will need 2-3 ultrasounds during that cycle. All reports can be faxed or emailed to your physician within 2-3 hours after the exam is finished.
To schedule an appointment
Please Call True Health Acupuncture at 702-475-0870
You can also book online on the True Health Acupuncture website.
1481 W Warm Spring Rd #129
Henderson, Nevada 89014
Testimonials
My name is Michelle Aukerman. And I just have to say that Joyce at True Health Acupuncture is probably the best ultrasound technician I have ever had in my life and I’ve been through several. She’s very personal and talks through everything and if something goes wrong, she says OK how do we make this right? What’s the next step we need to take? You don’t hear that from any other ultrasound tech, they're so jaded. The comfort environment at True Health Acupuncture is unmatchable. It does not feel like a doctor's office and everybody is so warm but when it comes to Joyce, she is completely unmatched. It’s like having your own mother right there with you. I highly highly recommend her.
Thank you, the Aukerman’s

Michelle A.
This is the second pregnancy that I came to Joyce for my outside monitoring. I have been very nervous about the whole process, but Joyce guided me through each and every ultrasound. Although the monitoring went smoothly, upon achieving pregnancy I developed some bleeding. Of course, I panicked. Joyce explained everything that was going on with my bleeding and helped me through this anxious time. I don’t know what I would have done without Joyce’s calm demeanor. And the added bonus is having acupuncture treatment right there at True Health Acupuncture, the office Joyce works out of. I will always be truly thankful for the amazing experience that I received from both Joyce and True Health to be a part of my fertility journey.

Sara P.
Joyce is an exceptional individual who made a significant impact during my IVF journey. I had the privilege of meeting her when I needed support, and she was able to perform ultrasounds when our IVF Dr was unable to accommodate us. Her ability to confirm our twin pregnancy was incredibly reassuring. Joyce took the time to explain everything she was observing, which not only made the experience more memorable but also helped alleviate my anxiety. Her compassionate approach truly made a difference in my experience.

Nicole B
IVF Trigger Shots and Luteal Phase Support – The Final Steps Before Pregnancy
Once the follicles have matured during stimulation, the next two steps are crucial for a successful IVF outcome: (1) triggering final oocyte maturation, and (2) supporting the uterine lining for implantation. Each stage involves carefully chosen medications that optimize success and reduce risk.
🔹 Trigger Injections – Signaling the Final Egg Maturation
The trigger shot mimics the body’s natural LH surge, signaling the final phase of egg development and preparing for retrieval ~36 hours later.
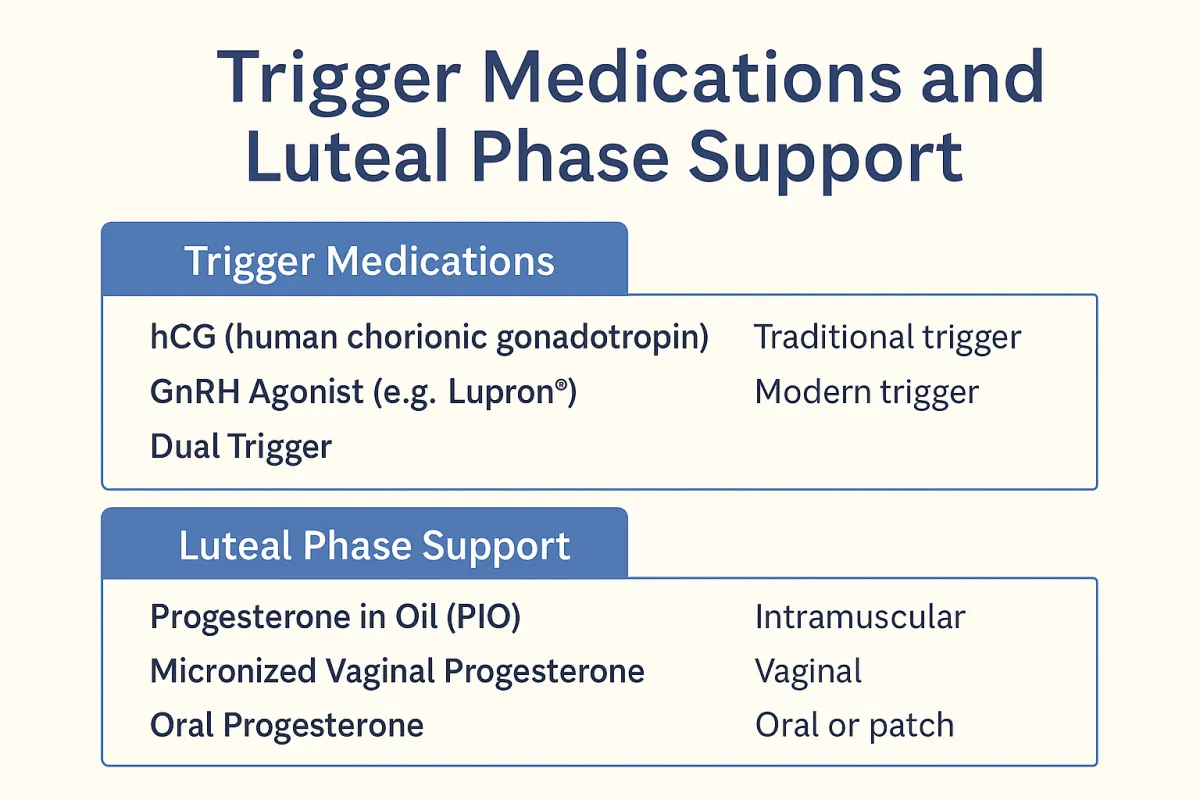
✅ Common Trigger Medications:
Medication Type Usage Notes hCG (human chorionic gonadotropin)Traditional trigger Pregnyl®, Novarel® (urinary); Ovidrel® (recombinant). Mimics LH, time-tested. GnRH Agonist (e.g., Lupron®)Modern trigger Causes the pituitary to release endogenous LH and FSH surge. Often used in antagonist protocols. Dual Trigger Combo of hCG + GnRH agonist Used in high responders or previous failed cycles to improve egg maturation while reducing OHSS risk.
⚠️ Important Considerations:
OHSS (Ovarian Hyperstimulation Syndrome): hCG increases OHSS risk in high responders (e.g., PCOS patients). A GnRH agonist is safer in these cases.
Trigger timing is critical — retrieval must occur ~36 hours after injection to avoid ovulation in vivo.
🔹 Luteal Phase Support – Holding the Uterine Lining
After the egg retrieval, the ovaries are no longer producing hormones at natural levels due to follicle aspiration. Luteal support replaces these missing signals to maintain a receptive endometrium for embryo transfer.
✅ Common Medications for Luteal Support:
Medication Route Brand Examples Notes Progesterone in Oil (PIO)Intramuscular Generic Gold standard; reliable absorption, but painful and inconvenient. Micronized Vaginal Progesterone Vaginal Endometrin®, Crinone® Less invasive; used widely in Europe and in some U.S. clinics. Oral Progesterone Oral Prometrium® Less commonly used due to inconsistent serum levels .Estradiol (E2)Oral or patch Estrace®, Vivelle-Dot® Used when estrogen support is needed alongside progesterone.
🔬 Protocol Duration:
Usually continues until the 10th–12th week of pregnancy, or until the placenta begins producing its own progesterone and estrogen (placental takeover).
Some clinics stop earlier if a natural LH surge occurred (e.g., in modified natural cycles).
🧬 Personalized Approaches
Luteal support is tailored based on:
Type of stimulation and trigger
Fresh vs. frozen transfer
Patient’s hormone levels
Clinic preference and evidence-based trends
Recent studies are also exploring subcutaneous progesterone, progesterone serum monitoring, and timed cessation based on early hCG rise.
✅ Summary
Phase Medications Purpose Trigger hCG, GnRH agonist, or both Induce final egg maturation Luteal Support Progesterone (IM, vaginal, or oral), Estradiol Maintain endometrial receptivity post-transfer