Ultrasound Monitorig
for Your IVF Cycle
For IVF monitoring cycles that are out-of-state of your location
Starting your cycle
Starting an IVF cycle is stressful enough, doing it with an out-of-state provider just increases that stress. That is why we have developed an out-of state monitoring program to help women that need ultrasound monitoring without having to travel to their provider. We follow your physicians instructions and with be able to accommodate your schedule. Most all cycles, whether retrievals or transfers, will need 2-3 ultrasounds during that cycle. All reports can be faxed or emailed to your physician within 2-3 hours after the exam is finished.
To schedule an appointment
Please Call True Health Acupuncture at 702-475-0870
You can also book online on the True Health Acupuncture website.
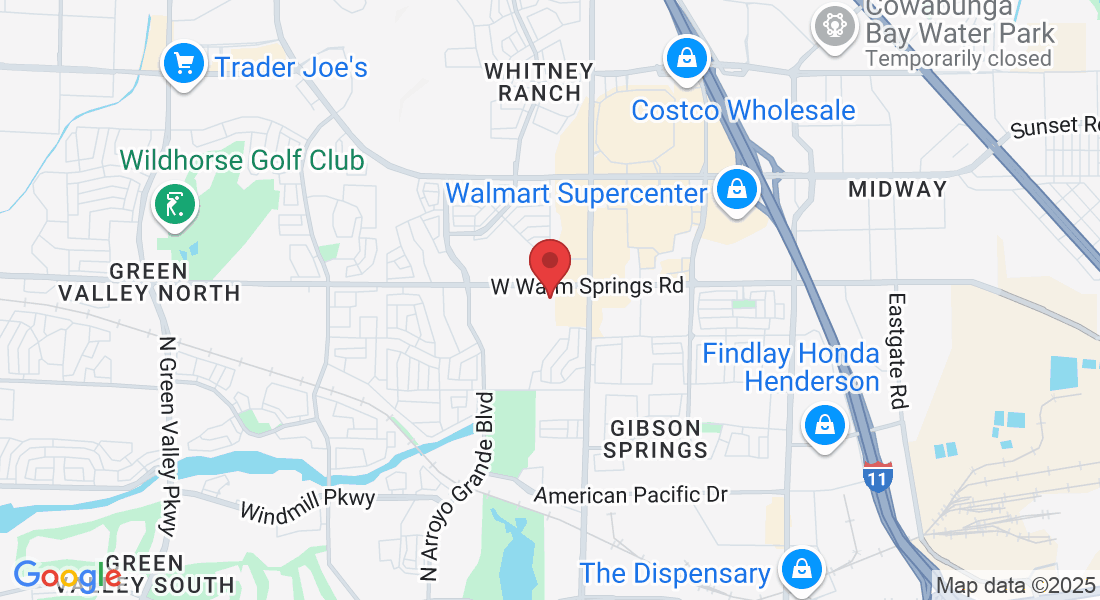
1481 W Warm Spring Rd #129
Henderson, Nevada 89014
Testimonials
My name is Michelle Aukerman. And I just have to say that Joyce at True Health Acupuncture is probably the best ultrasound technician I have ever had in my life and I’ve been through several. She’s very personal and talks through everything and if something goes wrong, she says OK how do we make this right? What’s the next step we need to take? You don’t hear that from any other ultrasound tech, they're so jaded. The comfort environment at True Health Acupuncture is unmatchable. It does not feel like a doctor's office and everybody is so warm but when it comes to Joyce, she is completely unmatched. It’s like having your own mother right there with you. I highly highly recommend her.
Thank you, the Aukerman’s

Michelle A.
This is the second pregnancy that I came to Joyce for my outside monitoring. I have been very nervous about the whole process, but Joyce guided me through each and every ultrasound. Although the monitoring went smoothly, upon achieving pregnancy I developed some bleeding. Of course, I panicked. Joyce explained everything that was going on with my bleeding and helped me through this anxious time. I don’t know what I would have done without Joyce’s calm demeanor. And the added bonus is having acupuncture treatment right there at True Health Acupuncture, the office Joyce works out of. I will always be truly thankful for the amazing experience that I received from both Joyce and True Health to be a part of my fertility journey.

Sara P.
Joyce is an exceptional individual who made a significant impact during my IVF journey. I had the privilege of meeting her when I needed support, and she was able to perform ultrasounds when our IVF Dr was unable to accommodate us. Her ability to confirm our twin pregnancy was incredibly reassuring. Joyce took the time to explain everything she was observing, which not only made the experience more memorable but also helped alleviate my anxiety. Her compassionate approach truly made a difference in my experience.

Nicole B

Asherman Syndrome: Understanding a Silent Reproductive Challenge
Asherman Syndrome: Understanding a Silent Reproductive Challenge
Asherman syndrome is a condition that affects the uterus, characterized by the formation of adhesions or scar tissue in the uterine cavity. Though not widely discussed, this condition can have significant implications for women's reproductive health. Named after Dr. Joseph Asherman who first described it in 1948, the syndrome deserves more attention in conversations about women's health.
What Causes Asherman Syndrome?
The primary cause of Asherman syndrome is trauma to the endometrium, the inner lining of the uterus. This trauma most commonly occurs following procedures such as:
Dilation and curettage (D&C), especially when performed for postpartum hemorrhage or miscarriage
Myomectomy (removal of uterine fibroids)
Cesarean section complications
Treatment of uterine infections
Endometrial ablation
Risk increases with multiple procedures, particularly when performed while the endometrium is vulnerable, such as after pregnancy.
Recognizing the Symptoms
Asherman syndrome often presents with:
Light or absent menstrual periods (hypomenorrhea or amenorrhea)
Recurrent pregnancy loss or infertility
Cyclical pelvic pain
Complications during pregnancy if conception occurs
Abnormal placentation in subsequent pregnancies
Some women may have the condition without obvious symptoms, discovering it only when facing fertility challenges.
Diagnosis and Treatment
Diagnosis typically involves:
Hysteroscopy (direct visualization of the uterine cavity)
Sonohysterography (ultrasound with saline infusion)
Hysterosalpingography (X-ray with contrast dye)
MRI in complex cases
Treatment aims to restore the normal uterine anatomy and function:
Surgical intervention through hysteroscopy to remove adhesions
Placement of devices like balloon catheters or IUDs to prevent re-adhesion
Hormonal therapy, typically estrogen, to promote endometrial regrowth
Antibiotics to prevent infection
Multiple procedures may be necessary in severe cases, and success rates vary depending on the extent of scarring.
Prevention and Awareness
The best approach to Asherman syndrome is prevention. This includes:
Careful technique during uterine procedures
Avoiding unnecessary intrauterine interventions
Prophylactic antibiotics when appropriate
Consideration of alternative management approaches for miscarriage
For women who have had uterine procedures, awareness of potential symptoms can lead to earlier diagnosis and intervention.
Living with Asherman Syndrome
Support groups and educational resources can help women navigate the emotional and physical challenges of this condition. While severe cases may impact fertility, advances in reproductive technology offer hope. Successful pregnancies are possible after treatment, though careful monitoring is essential.
For women experiencing unusual menstrual patterns after uterine procedures or struggling with unexplained fertility issues, discussing the possibility of Asherman syndrome with a reproductive specialist may be an important step toward resolution.
By increasing awareness of this condition, we can help ensure that women receive timely diagnosis and appropriate care for this treatable but often overlooked syndrome.
Pregnancy After Asherman Syndrome: A Closer Look
For women diagnosed with Asherman Syndrome, fertility concerns are often at the forefront of their minds. The ability to conceive and carry a pregnancy to term depends significantly on several factors, particularly the severity of intrauterine adhesions and the success of treatment.
Pregnancy Success Rates
As shown in the chart, pregnancy outcomes vary considerably based on the severity of adhesions:
Mild Cases: Women with mild adhesions have the most favorable prognosis, with approximately 85% achieving conception and 75% having successful live births after treatment.
Moderate Cases: Those with moderate adhesions can expect around 70% conception rates and 55% live birth rates following appropriate interventions.
Severe Cases: Women with extensive adhesions face more significant challenges, with only about 35% achieving pregnancy and 25% having successful live births even after treatment.
Overall, across all severity levels, about 65% of women with treated Asherman Syndrome will conceive,
with approximately 55% ultimately having successful pregnancies.

Factors Influencing Pregnancy Success
Several key factors influence reproductive outcomes:
Location of adhesions: Adhesions near the fallopian tube openings or covering a large portion of the endometrial surface have more significant impacts on fertility.
Endometrial function: The quality and thickness of the remaining endometrium after treatment is crucial for embryo implantation.
Treatment expertise: Outcomes are significantly better when procedures are performed by specialists experienced in treating Asherman Syndrome.
Age and other fertility factors: As with all fertility issues, additional factors like age, ovarian reserve, and partner's fertility also play important roles.
Pregnancy Considerations
Women who do conceive after Asherman Syndrome treatment should be considered high-risk and require specialized prenatal care due to:
Placental attachment issues: Higher risk of placenta accreta, increta, or percreta
Miscarriage risk: Elevated rates of early pregnancy loss
Preterm labor: Increased likelihood of premature delivery
Growth restriction: Higher incidence of intrauterine growth restriction
Early consultation with reproductive endocrinologists who specialize in Asherman Syndrome provides the best chance for successful pregnancy outcomes, as timely and expert intervention can significantly improve the prognosis for women hoping to build their families after this diagnosis.