Ultrasound Monitorig
for Your IVF Cycle
For IVF monitoring cycles that are out-of-state of your location
Starting your cycle
Starting an IVF cycle is stressful enough, doing it with an out-of-state provider just increases that stress. That is why we have developed an out-of state monitoring program to help women that need ultrasound monitoring without having to travel to their provider. We follow your physicians instructions and with be able to accommodate your schedule. Most all cycles, whether retrievals or transfers, will need 2-3 ultrasounds during that cycle. All reports can be faxed or emailed to your physician within 2-3 hours after the exam is finished.
To schedule an appointment
Please Call True Health Acupuncture at 702-475-0870
You can also book online on the True Health Acupuncture website.
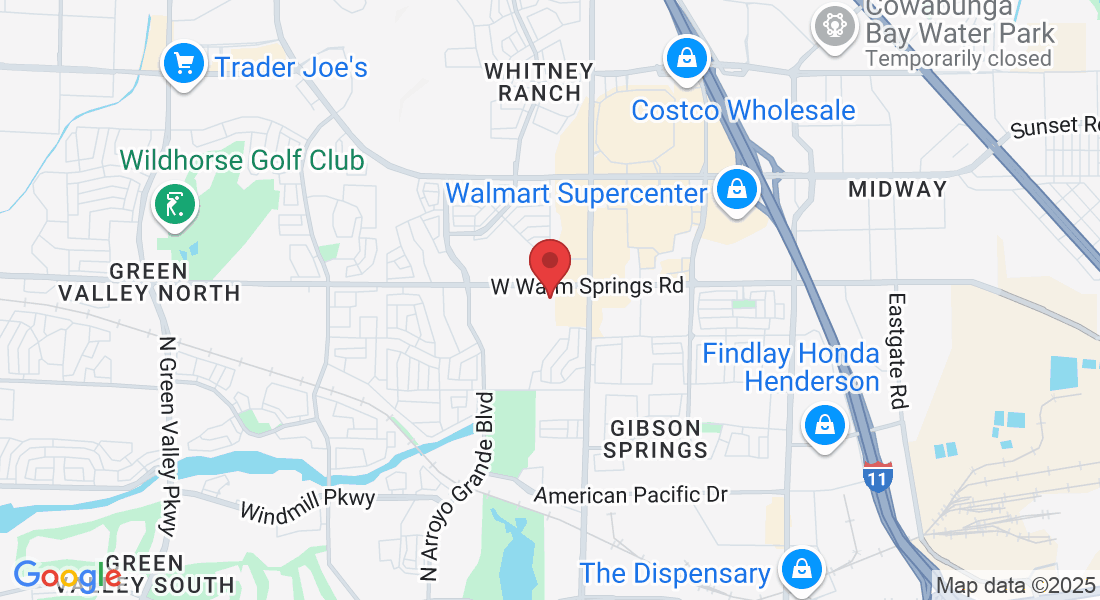
1481 W Warm Spring Rd #129
Henderson, Nevada 89014
Testimonials
My name is Michelle Aukerman. And I just have to say that Joyce at True Health Acupuncture is probably the best ultrasound technician I have ever had in my life and I’ve been through several. She’s very personal and talks through everything and if something goes wrong, she says OK how do we make this right? What’s the next step we need to take? You don’t hear that from any other ultrasound tech, they're so jaded. The comfort environment at True Health Acupuncture is unmatchable. It does not feel like a doctor's office and everybody is so warm but when it comes to Joyce, she is completely unmatched. It’s like having your own mother right there with you. I highly highly recommend her.
Thank you, the Aukerman’s

Michelle A.
This is the second pregnancy that I came to Joyce for my outside monitoring. I have been very nervous about the whole process, but Joyce guided me through each and every ultrasound. Although the monitoring went smoothly, upon achieving pregnancy I developed some bleeding. Of course, I panicked. Joyce explained everything that was going on with my bleeding and helped me through this anxious time. I don’t know what I would have done without Joyce’s calm demeanor. And the added bonus is having acupuncture treatment right there at True Health Acupuncture, the office Joyce works out of. I will always be truly thankful for the amazing experience that I received from both Joyce and True Health to be a part of my fertility journey.

Sara P.
Joyce is an exceptional individual who made a significant impact during my IVF journey. I had the privilege of meeting her when I needed support, and she was able to perform ultrasounds when our IVF Dr was unable to accommodate us. Her ability to confirm our twin pregnancy was incredibly reassuring. Joyce took the time to explain everything she was observing, which not only made the experience more memorable but also helped alleviate my anxiety. Her compassionate approach truly made a difference in my experience.

Nicole B
🔍 IVF: The Road to Success Wasn’t Easy
🔍 IVF: The Road to Success Wasn’t Easy
The Early Challenges and Controversies of In Vitro Fertilization
After the historic birth of Louise Brown in 1978, IVF was hailed as a miracle by some—and criticized as unnatural by others. The journey from scientific experiment to trusted medical treatment wasn’t smooth. Let’s look at the struggles, skepticism, and ethical debates that shaped IVF in its early years.
🧪 The Science Was Fragile
In the 1970s and early 1980s:
Egg retrieval required surgery, since ultrasound-guided aspiration didn’t yet exist.
Embryo culture techniques were primitive, relying on basic nutrients and uncertain lab conditions.
Success rates were extremely low—often less than 5% per cycle.
Even small changes in temperature or lab handling could damage the embryo. IVF was still experimental, and many patients underwent it with no guarantee of success.
⚖️ The Ethics Were Debated
Many questioned whether fertilizing human eggs in a lab was ethical. Concerns included:
Was this “playing God”?
What would happen to unused embryos?
Could this lead to designer babies?
In 1984, the Warnock Report in the UK addressed these issues and helped establish the first ethical guidelines for IVF. It led to the creation of the Human Fertilisation and Embryology Authority (HFEA) in 1990—the first regulatory body of its kind in the world.
🏥 Limited Access & High Costs
In its early years, IVF was:
Only available at a few select clinics
Extremely expensive
Not covered by insurance
This made IVF accessible mainly to wealthier families, raising concerns about inequality in reproductive care.
🧬 But Progress Was Fast
Despite the criticism, progress came quickly:
Ultrasound-guided egg retrieval replaced surgery.
Hormonal stimulation protocols improved egg yield.
Cryopreservation (freezing embryos) became a game-changer.
By the late 1980s, IVF had improved dramatically, with success rates climbing and more clinics offering it worldwide.
🔬 IVF Breakthroughs: How Progress Was Made After 1978
The birth of Louise Brown in 1978 was just the beginning. What followed was a series of scientific leaps that turned IVF from a risky experiment into a trusted fertility treatment used around the world today.
Here’s how the progress unfolded:
🧫 1. Improved Egg Retrieval Methods
Then:
In the earliest IVF attempts, eggs were collected through open abdominal surgery—a painful and invasive process requiring hospitalization.
Now:
By the early 1980s, doctors started using transvaginal ultrasound-guided aspiration, a much less invasive procedure that allows precise egg retrieval using a thin needle.
🔍 Why it mattered:
It reduced recovery time, improved egg yield, and made IVF safer and more widely accessible.
💉 2. Refined Hormonal Stimulation Protocols
Then:
Early IVF cycles relied on natural ovulation, meaning doctors waited for a woman to release one egg—greatly reducing success rates.
Now:
Doctors use gonadotropins (like FSH and LH) to stimulate the ovaries to produce multiple mature eggs in one cycle.
📈 Why it mattered:
More eggs = more embryos = more chances of pregnancy and better options for freezing.
🧪 3. Advanced Culture Media for Embryo Growth
Then:
Early embryo culture media were basic and not optimized for human embryos, which could limit embryo viability.
Now:
Scientists have developed specialized media that support embryo development from fertilization to the blastocyst stage (day 5-6).
🌱 Why it mattered:
Healthier embryos and the ability to grow them longer in the lab led to better selection for transfer—and higher pregnancy rates.
🧊 4. Cryopreservation: Freezing Embryos
Then:
If embryos weren't transferred immediately, they were lost—freezing methods often damaged them.
Now:
Modern vitrification (a flash-freezing method) preserves embryos, eggs, and even ovarian tissue with very high survival rates.
🧬 Why it mattered:
Couples can freeze extra embryos for future use, reducing the need for multiple stim cycles and making IVF more cost-effective over time.
🧬 5. ICSI: Intracytoplasmic Sperm Injection (1992)
Then:
Fertilization relied on sperm naturally penetrating the egg, which didn’t work well in severe male infertility cases.
Now:
With ICSI, a single sperm is injected directly into the egg.
👨🔬 Why it mattered:
ICSI revolutionized IVF for couples dealing with male factor infertility—allowing fertilization even with very low sperm counts or motility.
🧫 6. Genetic Testing (PGT-A, PGT-M)
Then:
All embryos looked alike under the microscope. There was no way to know which were genetically normal.
Now:
Preimplantation genetic testing (PGT) allows screening for chromosomal abnormalities or specific diseases before embryo transfer.
🧠 Why it mattered:
This helps reduce miscarriage risk and improve success rates, especially in older women or those with recurrent loss.
🌍 7. Wider Access, Better Regulations
Over time, IVF moved from private labs to regulated fertility centers and academic hospitals. Most countries have developed ethical guidelines and licensing bodies (like the HFEA in the UK and CDC/SART reporting in the US) to monitor practices.
📚 Why it mattered:
Patients now have transparency, ethical safeguards, and standardized care.
In Summary
Progress in IVF didn’t happen all at once. It came in stages—bit by bit—through better tools, smarter science, and deeper understanding of human reproduction. Today’s IVF success rates are over 40–60% per transfer for many age groups, compared to under 10% in the early 1980s.