Ultrasound Monitorig
for Your IVF Cycle
For IVF monitoring cycles that are out-of-state of your location
Starting your cycle
Starting an IVF cycle is stressful enough, doing it with an out-of-state provider just increases that stress. That is why we have developed an out-of state monitoring program to help women that need ultrasound monitoring without having to travel to their provider. We follow your physicians instructions and with be able to accommodate your schedule. Most all cycles, whether retrievals or transfers, will need 2-3 ultrasounds during that cycle. All reports can be faxed or emailed to your physician within 2-3 hours after the exam is finished.
To schedule an appointment
Please Call True Health Acupuncture at 702-475-0870
You can also book online on the True Health Acupuncture website.
1481 W Warm Spring Rd #129
Henderson, Nevada 89014
Testimonials
My name is Michelle Aukerman. And I just have to say that Joyce at True Health Acupuncture is probably the best ultrasound technician I have ever had in my life and I’ve been through several. She’s very personal and talks through everything and if something goes wrong, she says OK how do we make this right? What’s the next step we need to take? You don’t hear that from any other ultrasound tech, they're so jaded. The comfort environment at True Health Acupuncture is unmatchable. It does not feel like a doctor's office and everybody is so warm but when it comes to Joyce, she is completely unmatched. It’s like having your own mother right there with you. I highly highly recommend her.
Thank you, the Aukerman’s

Michelle A.
This is the second pregnancy that I came to Joyce for my outside monitoring. I have been very nervous about the whole process, but Joyce guided me through each and every ultrasound. Although the monitoring went smoothly, upon achieving pregnancy I developed some bleeding. Of course, I panicked. Joyce explained everything that was going on with my bleeding and helped me through this anxious time. I don’t know what I would have done without Joyce’s calm demeanor. And the added bonus is having acupuncture treatment right there at True Health Acupuncture, the office Joyce works out of. I will always be truly thankful for the amazing experience that I received from both Joyce and True Health to be a part of my fertility journey.

Sara P.
Joyce is an exceptional individual who made a significant impact during my IVF journey. I had the privilege of meeting her when I needed support, and she was able to perform ultrasounds when our IVF Dr was unable to accommodate us. Her ability to confirm our twin pregnancy was incredibly reassuring. Joyce took the time to explain everything she was observing, which not only made the experience more memorable but also helped alleviate my anxiety. Her compassionate approach truly made a difference in my experience.

Nicole B
🧪 Before IVF: The Tests and Treatments That Often Come First
🔄 How IVF Evolved: From One Procedure to Many Options
IVF didn’t stop evolving after Louise Brown’s birth in 1978—it exploded into a whole new world of fertility care. Over the decades, IVF has branched out into different paths, new tools, and tailored treatments, giving millions of people around the world hope for a family.
Here’s how IVF evolved—and what it looks like today.
🔬 1. From One Embryo to Personalization
Then:
In early IVF cycles, doctors transferred multiple embryos at once, hoping at least one would implant. This often led to high-risk multiple pregnancies (twins, triplets, or more).
Now:
Thanks to better embryo grading and preimplantation genetic testing (PGT-A), doctors often transfer just one high-quality embryo (single embryo transfer or SET). This reduces risks and improves outcomes.
✅ Takeaway: IVF is now more precise—success rates have gone up even with fewer embryos transferred.
🧬 2. From IVF to ICSI and Beyond
The development of intracytoplasmic sperm injection (ICSI) in the 1990s revolutionized how sperm and egg were combined. Instead of mixing sperm in a dish and hoping one fertilizes the egg, a single sperm is injected directly into the egg.
Why it matters:
ICSI opened the door for men with very low sperm counts or poor motility to still become biological fathers.
🧊 3. From Fresh-Only to Frozen Flexibility
In the early days, only fresh embryos were used—and if implantation failed, the whole cycle had to be repeated.
Now, with vitrification (a fast-freezing technique), embryos, eggs, and even ovarian tissue can be preserved for future use without damage.
📦 Frozen embryo transfers (FETs) have become standard and often result in equal or higher success rates than fresh transfers.
🏳️🌈 4. Expanding Access: IVF for All Family Types
Originally, IVF was mainly used by heterosexual couples dealing with infertility. But that’s changed.
Today, IVF supports:
Single parents by choice
LGBTQ+ families (using donor sperm, donor eggs, and gestational carriers)
Fertility preservation for cancer patients or those delaying parenthood (egg/sperm freezing)
🌍 IVF has become a tool for inclusive family-building, not just infertility.
⚖️ 5. Global Reach and Regulation
IVF is now practiced in nearly every developed country, and many developing ones, too. While regulations vary, most countries have guidelines for safety, embryo limits, donor anonymity, and ethical concerns.
📊 Global ART Registries now track success rates, helping patients make informed decisions about clinics and treatments.
💡 Bonus Evolution: IVF + AI & Data Science
Newer innovations include:
Artificial intelligence to select the best embryos
Wearable hormone sensors for monitoring cycles
Genetic profiling to personalize stimulation protocols
The future of IVF might look even more data-driven, non-invasive, and personalized than we ever imagined.
✨ IVF Today = Options, Empowerment, and Hope
From one experimental embryo in 1978 to millions of births worldwide, IVF has come a long way. Today, patients can choose the approach that fits their biology, values, and goals. It’s no longer one-size-fits-all—it’s tailored reproductive medicine.
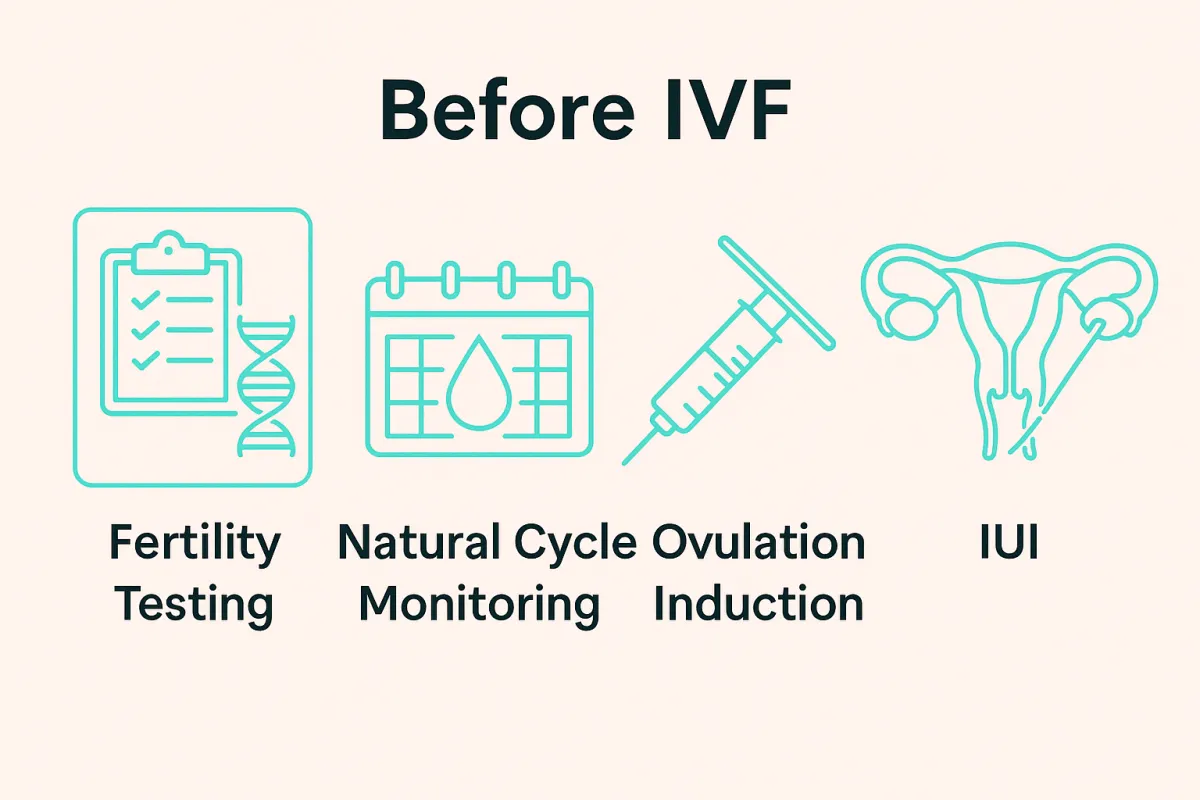
🧪 Before IVF: The Tests and Treatments That Often Come First
IVF might be the most well-known fertility treatment, but it's rarely the first step. Before you get to embryo labs and transfer dates, there’s an entire process designed to evaluate your reproductive health and determine the least invasive, most effective path to pregnancy.
Let’s explore what usually happens before IVF is recommended.
🔍 Step 1: Basic Fertility Testing for Both Partners
Before jumping into treatment, most fertility clinics will run a series of evaluations to identify possible causes of infertility:
🧬 For Women:
Hormonal panel (Day 3 bloodwork): FSH, LH, Estradiol, AMH (Anti-Müllerian Hormone) to assess ovarian reserve.
Thyroid and prolactin levels: Imbalances here can affect ovulation.
Transvaginal ultrasound: To check for ovarian follicles, fibroids, or polyps.
HSG (Hysterosalpingogram): An X-ray test to see if the fallopian tubes are open.
Saline Sonogram (SIS): A fluid-based ultrasound to assess the uterine lining.
🧬 For Men:
Semen analysis: Evaluates sperm count, motility, morphology (shape), and volume.
In some cases: DNA fragmentation tests or hormone labs (like testosterone, FSH, LH).
🧠 Why it matters: These tests help identify underlying issues like PCOS, endometriosis, male factor infertility, or tubal blockages—each requiring a different treatment approach.
🌀 Step 2: Natural Cycle Monitoring (Especially for Irregular Cycles)
For women with irregular periods, the first step is often cycle monitoring to track ovulation patterns without medication. This can include:
Serial ultrasounds: To track follicle growth
Blood tests: To monitor rising hormone levels (LH, progesterone, estrogen)
Ovulation predictor kits (OPKs) or at-home monitors
🌿 Doctors may try natural timed intercourse cycles or prescribe ovulation induction meds (like Clomid or Letrozole) to help regulate the cycle.
💉 Step 3: IUI – Intrauterine Insemination
If ovulation tracking and timed intercourse don’t work, many couples try IUI (Intrauterine Insemination) before IVF.
How IUI works:
A woman is monitored for ovulation (either naturally or with medication).
At peak ovulation, washed and concentrated sperm is placed directly into the uterus using a thin catheter.
It’s quick, usually painless, and takes less than 10 minutes.
🧠 IUI is often used for:
Unexplained infertility
Mild male factor infertility
Cervical issues
LGBTQ+ family building using donor sperm
📈 Success rates vary by age but typically range from 10–20% per cycle.
⚙️ When IVF Becomes the Next Step
IVF is usually recommended when:
IUI has failed after 3–6 cycles
There are blocked fallopian tubes
There is severe male factor infertility
The woman has low ovarian reserve
There’s a need for genetic testing or embryo banking
LGBTQ+ families need both egg/sperm donation and surrogacy
📝 Summary: IVF Isn’t the First Step—It’s the Best Next Step for Some
Modern fertility care is stepwise and personalized. Most people go through testing and less invasive treatments like ovulation tracking and IUI before moving on to IVF.
Understanding these early phases helps patients: ✅ Make informed decisions
✅ Feel empowered during the process
✅ Avoid jumping to IVF before it’s truly necessary